Person Centred Care – An Introduction
“It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.” William Osler
“This porridge is too hot!” she exclaimed.
So, she tasted the porridge from the second bowl.
“This porridge is too cold,” she said
So, she tasted the last bowl of porridge.
“Ahhh, this porridge is just right,” she said happily and she ate it all up.
A special room
There is a special room in the medical home for the practice of ‘person centred care’.
We know that many people miss out on important medical treatments. The care they receive is ‘too cold’.
However, there is also a growing recognition that many of our patients are put in harms way by too much therapeutic intervention.
Too-hot care
‘Too-hot’ care can come in a number of forms.
Some treatments or operations sound good – but just don’t work.
“One of the first duties of the physician is to educate the masses not to take medicine” – William Osler
A treatment may be accepted wisdom, pased down from an authorative source. It may sound like a good idea based on a postulated mechanism of action, or by its effect on a surrogate biochemical marker.
However,the treatment may make no difference on outcomes that matter to people. Or it may even make things worse.
Ezetimbe when used with Simvastatin for patients with familial hypercholesterolaemia lowered LDL more than Simvastatin alone. it was therefore effective against a surrogate marker. However, it did not demonstrate any benefit on cardiac events. (in fact, it trends towards causing more infarcts and deaths)
ENHANCE Study http://www.pubmed.org/18376000
We fail to ‘abandon ship’ despite the rising waters
“One special advantage of the skeptical attitude of mind is that a man is never vexed to find that after all he has been in the wrong.” William Osler
Sometimes a treatment may have demonstrated effectiveness in a clinical trial, but later trials or systematic reviews do not replicate those benefits. In a recent paper, Vinay Prasad reviewed 363 articles in the NEJM ‘that tested something that doctors were doing at that time’, and found that 40% of articles ‘concluded that what we were doing was no better or even worse than not doing it…That is, 40% of articles were medical reversals.’
‘When a common belief is contradicted with a better study, how long does it take before people stop citing the original incorrect belief? About 10 years. There is an inertia to contradicted practices. It’s a lot harder to stop doing something that you are used to doing, that you believe works, even in the face of really overwhelming evidence that it’s ineffective, that it doesn’t work’
Health Report RN 29/7/2013
http://www.abc.net.au/radionational/programs/healthreport/reversal-of-established-medical-practice/4850000#transcript
Reversals of Established Medical Practices – Evidence to Abandon Ship Vinay Prasad, MD; Adam Cifu, MD; John P. A. Ioannidis, MD, DSc JAMA. 2012;307(1):37-38. doi:10.1001/jama.2011.1960.
Guidelines look at average patients, not individual patients
Sometimes there may be some potential benefit of a treatment for an ‘average’ patient. But is the patient in front of you ‘average’. Does she have other conditions that mitigate the benefits, or is she taking other medications that increase her risk of adverse outcomes? Do we even know if the proposed treatment has been tested on patients like her?
In addition to clinical considerations, different people have different values, experiences, resources, and differing appetite for risk – all of which will influence their treatment decisions.
The Burden of Treatment is often not considered
All of our interventions require some disruption to the normal lives of our patients. The ‘burden of treatment’ is the negative effects that our recommendations have on our patients’ quality of life. These include opportunity costs in time, money, and focus, and a decreased sense of well being . Sometimes it is worth it – sometimes it isn’t.
The present good quality evidence indicates that regular self‐ monitoring of blood glucose in type 2 diabetics not on insulin gives no benefits, is not cost‐effective and may have negative consequences (like worsening on depression scales).
Tools for Practice http://www.acfp.ca/Portals/0/docs/TFP/20111028_112201.pdf
We overdiagnose illness
There is the burden of ‘overdiagnosis’. As we increasingly focus on screening and risk factor identification, we run the additional risk of labelling our patients with a new diagnosis for a condition that would have no significant impact on their quality of life if it was never diagnosed. Our increasingly sensitive imaging picks up ‘incidentalomas’ at higher rates, and ‘experts’ lower the threshold at which a test result falls in the ‘normal’ range.
Despite increased detection of breast, thyroid and prostate cancers over recent decades, there has not been a corresponding benefit in mortality rates. Gestational Diabetes, ADHD, and Vit D deficiency are examples where the number of diagnosed sufferers has increased because the definition of normal has changed.
We do things that don’t change our management
Finally, we commonly order investigations that make no difference to our management, exposing our patients to waste or potential harm.
If a patient is on treatment for established osteoporosis, what is the value of annual bone density scans? Cholesterol results change very little in an individual – what is the rationale for annual testing?
Swimming against the stream
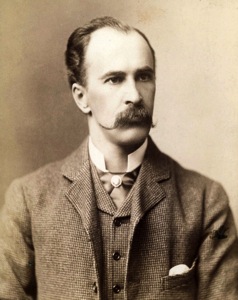 “The young physician starts life with 20 drugs for each disease, and the old physician ends life with one drug for 20 diseases.” William Osler
“The young physician starts life with 20 drugs for each disease, and the old physician ends life with one drug for 20 diseases.” William Osler
As clinicians become more experienced, the more they value a ‘healthy scepticism’ about therapeutics. Don’t be the first to use a new drug, but don’t be the last.
We often feel that we are swimming against the stream when we caution our patents against having a test or undergoing a treatment or operation, especially if that investigation or treatment is recommended by a specialist colleague. The easier option is to go with the flow.
However, in the medical home we are accountable to our patients for their comprehensive health. We are responsible for protecting them from harm and waste.
It strengthens our confidence to swim against the stream on behalf of the patient in front of us if we stand beside a respected cohort of colleagues with whom we have examined the evidence around a clinical question.
Shared Decision Making
Shared decision making is the process whereby we help people come to their own conclusions on what they would like to do. We aim to provide them with the information they need to make informed decisions about the care they receive, bassd on their individual circumstances, values and resources.
The Person Centred Care Collaboration
The ‘Person Centred Care Collaboration’ of the Australian Centre for the Medical Home aims to bring clinicians together to discuss the evidence around interventions that may be ‘too hot’ or ‘too cold’. It will collate and share resources that aid shared decision making’ with our patients.
This ‘goldilocks’ approach to therapeutics – getting it just right- has a number of names, including ‘Minimally disruptive medicine’ and ‘Lean medicine’. It is related to the POEMs movement – ‘Patient Orientated Evidence that Matters’. It is informed by international groups such as the Cochrane Collaboration, the Dartmouth Institute, the Mayo Clinic, the Alberta College of Family Physicians, the Therapeutics Education Collaborative, the National Centre for Clinical Excellence, and the newly established Patient Centred Outcomes Research Institute. In Australia, we draw on the National Prescribng Service and the Centre for Resaerch in Evidence Based Practice.
http://www.bmj.com/content/339/bmj.b2803
http://shareddecisions.mayoclinic.org/
http://minimallydisruptivemedicine.org/
http://therapeuticseducation.org/podcast/episode-superlative-minimally-disruptive-podcast-victor-montori
What would you do, doctor?
The Person Centred Care Collaboration will build a bower of answers to clinical questions that are important to our patients by ‘stealing shamelessly’ from the evidence gathered by others.
Members will be invited to submit questions, and to participate in discussion about of the evidence. Other members We will also collect resources that aid decision making by patients and their clinicians.
- Who should have a Vitamin D test, and how do we act on the results?
- What is the evidence for outcomes that matter in the management of diabetes?
- How relevant is Cholesterol measurement in the management of cardiovascular disease?
- When should we un-prescribe medicines?
- Should we support the guidelines that recommend Omega 3 supplementation? CoEnzymeA? Glucosamine?
- Should I have that back operation?
Collegiality
The Person Centred Care Collaboration values independence, transparency, agility and collegaility. Practising Person Centred Care is not a ‘soft’ science. It is rigorous – as ‘hard as nails’ – in understanding the evidence.
We will build our bower at http://personcentredcare.org. You are invited to sign on as a member.